What Are Piles? Causes, Symptoms & Treatment Options
Piles, medically referred to as hemorrhoids, are swollen and inflamed veins located in the lower rectum and anal region. This condition is common and can affect individuals of different age groups due to lifestyle habits, bowel patterns, and physical strain. In Thrissur, many people seek clear information about piles to understand the condition, recognize early symptoms, and adopt suitable preventive and management measures. Although piles are not usually dangerous, they can cause discomfort and interfere with daily activities if not addressed properly.
Piles develop gradually and may remain mild in the early stages. However, without appropriate care and lifestyle adjustments, the condition can progress and lead to persistent symptoms. Understanding piles in detail helps individuals make informed decisions about personal health and long-term well-being.
1. Understanding the Anatomy of Piles
The anal canal contains a network of blood vessels that assist in maintaining bowel control and supporting normal defecation. These blood vessels are naturally present and function as cushions that help regulate pressure during bowel movements. When these veins are exposed to repeated strain or pressure, they can enlarge and become swollen, forming hemorrhoids.
Increased pressure in the lower rectum is the primary factor responsible for the development of piles. This pressure weakens the vein walls over time, causing them to stretch and bulge. The condition may develop slowly and often remains unnoticed until symptoms become more prominent.
2. Types of Piles (Hemorrhoids)
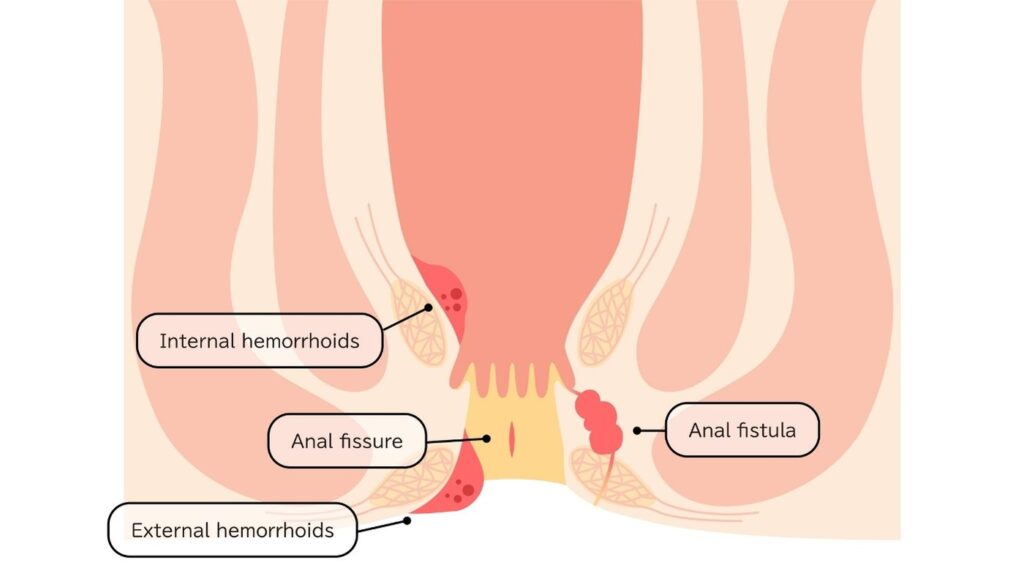
Piles are broadly categorized based on their location within or outside the anal canal. Each type presents different characteristics and symptoms.
Internal Hemorrhoids
Internal hemorrhoids develop inside the rectum and are usually painless because this area contains fewer pain-sensitive nerves. However, they can cause bleeding during bowel movements. In some cases, internal hemorrhoids may protrude outside the anus, a condition known as prolapse, which can lead to irritation and discomfort.
External Hemorrhoids
External hemorrhoids form under the skin around the anus. These are more likely to cause pain, swelling, itching, and tenderness. External hemorrhoids may also develop blood clots, resulting in a condition known as thrombosed hemorrhoids, which can be particularly uncomfortable.
Both internal and external hemorrhoids may occur simultaneously, depending on individual risk factors and lifestyle habits.
3. Common Causes of Piles
Several factors contribute to the formation of piles. These causes are often related to daily routines, physical strain, and digestive health.
Chronic Constipation
Frequent straining during bowel movements places excessive pressure on rectal veins. Hard stools also increase friction and irritation in the anal canal, raising the risk of hemorrhoid development.
Prolonged Sitting
Sitting for extended periods, especially on the toilet, can increase pressure in the anal area. Reduced blood circulation in this region may further contribute to vein swelling.
Pregnancy
During pregnancy, hormonal changes and increased pressure from the growing uterus can affect blood flow in the pelvic region. This makes pregnant individuals more susceptible to hemorrhoids.
Obesity
Excess body weight adds pressure to the pelvic and rectal veins. This increased strain may accelerate the development of piles and worsen existing symptoms.
Low-Fiber Diet
A diet low in fiber can result in hard stools and irregular bowel movements. Fiber plays a key role in maintaining stool softness and preventing constipation.
Aging
As people age, the supportive tissues around rectal veins may weaken. This natural process increases vulnerability to hemorrhoid formation.
4. Symptoms of Piles
The symptoms of piles vary depending on the type and severity of the condition. Some individuals may experience mild discomfort, while others may have more noticeable signs.
Rectal Bleeding
One of the most common symptoms is bright red blood during or after bowel movements. The bleeding is usually painless and may appear on toilet paper or in the toilet bowl.
Itching and Irritation
Inflamed hemorrhoids can cause persistent itching and irritation around the anal area. This may worsen after bowel movements or prolonged sitting.
Pain and Discomfort
External hemorrhoids often cause pain, particularly during sitting or bowel movements. Thrombosed hemorrhoids may lead to sudden and intense pain.
Swelling or Lumps
Swollen veins may form visible or palpable lumps around the anus. These lumps may feel soft or firm depending on the presence of blood clots.
Mucus Discharge
Some individuals may experience mucus discharge, which can contribute to irritation and discomfort.
Recognizing these symptoms early helps reduce the risk of complications and allows for timely management.
5. Stages of Internal Hemorrhoids
Internal hemorrhoids are commonly classified into stages based on their severity and degree of prolapse.
Stage One
Hemorrhoids remain inside the rectum and may cause bleeding without visible protrusion.
Stage Two
Hemorrhoids protrude outside the anus during bowel movements but return inside on their own.
Stage Three
Hemorrhoids protrude and require manual repositioning back into the rectum.
Stage Four
Hemorrhoids remain permanently outside the anus and cannot be pushed back. This stage may cause persistent discomfort and complications.
Understanding these stages helps determine appropriate management strategies.
6. Diagnosis of Piles
Diagnosis of piles typically begins with a review of symptoms and a physical examination. Visual inspection and digital rectal examination are commonly used to assess external and internal hemorrhoids.
In some cases, additional diagnostic procedures such as anoscopy, sigmoidoscopy, or colonoscopy may be recommended. These tests help rule out other causes of rectal bleeding and evaluate the condition of the lower digestive tract. Accurate diagnosis ensures appropriate treatment planning and reduces the risk of misinterpretation.
7. Possible Complications of Untreated Piles
When piles are left unmanaged, complications may develop over time.
Anemia
Chronic blood loss from hemorrhoids can result in anemia, leading to fatigue and weakness.
Thrombosis
Blood clots may form in external hemorrhoids, causing sudden pain and swelling.
Strangulated Hemorrhoids
Prolapsed hemorrhoids may lose blood supply, resulting in severe pain and tissue damage.
Infection
Although uncommon, infected hemorrhoids can occur and may require medical attention.
Timely management helps reduce the likelihood of these complications.
8. Prevention of Piles
Preventive measures focus on maintaining healthy bowel habits and reducing pressure on rectal veins.
Maintain a Fiber-Rich Diet
Consuming fiber-rich foods promotes regular bowel movements and reduces the risk of constipation.
Stay Hydrated
Adequate fluid intake helps soften stools and supports digestive health.
Practice Proper Bathroom Habits
Avoid straining and do not delay bowel movements. Responding promptly to the urge to pass stool reduces pressure on the anal area.
Engage in Regular Physical Activity
Exercise helps maintain healthy digestion, improves circulation, and supports weight management.
Avoid Prolonged Sitting
Taking breaks from sitting and using supportive seating arrangements can reduce strain on the rectal region.
9. When to Seek Medical Evaluation
Medical evaluation is recommended when symptoms persist, bleeding continues, or pain becomes severe. Rectal bleeding should always be taken seriously, as it may indicate conditions other than hemorrhoids.
Individuals experiencing prolapsed hemorrhoids, recurrent symptoms, or discomfort that does not improve with basic care should seek professional assessment for appropriate guidance.
10. Living With Piles
Living with piles involves adopting healthy habits and making consistent lifestyle adjustments. Many individuals manage symptoms effectively through dietary improvements, proper hydration, and regular physical activity.
Awareness of triggers and early symptom recognition allows individuals to take prompt action and prevent recurrence. Maintaining long-term bowel health plays a significant role in improving comfort and quality of life.
11. Final Thought
Piles, or hemorrhoids, are a common condition caused by increased pressure on rectal veins and influenced by lifestyle and dietary factors. They may present with symptoms such as bleeding, pain, itching, and swelling. With early recognition, proper management, and preventive measures, most individuals can effectively control symptoms and reduce the risk of recurrence. For individuals seeking information in Thrissur, understanding piles supports informed health decisions and encourages timely care when needed.
Table Of Content
Candidates
Good candidates are individuals with persistent symptoms such as bleeding, pain, or prolapse that do not improve with conservative management. Learn more
Cost
The cost of piles treatment in Thrissur varies depending on the treatment method, disease severity, hospital facilities, and postoperative care needs. Learn more
Consultation
During the consultation, the doctor evaluates symptoms, performs a clinical examination, reviews medical history, and discusses suitable treatment options. Learn more
Questions
You should ask about treatment methods, recovery time, possible risks, expected results, and follow-up care. Learn more
Risks and safety
Piles treatment is generally safe when properly performed, though risks may include pain, bleeding, infection, or recurrence. Learn more
Preparation
Preparation includes medical evaluation, medication adjustments, dietary guidance, bowel preparation if required, and planning postoperative care. Learn more
Steps
The procedure typically includes anesthesia, removal or reduction of hemorrhoidal tissue, bleeding control, and postoperative monitoring. Learn more
Recovery
Recovery usually involves gradual pain reduction, wound healing, bowel habit regulation, and return to daily activities over time. Learn more
Results
Results often include relief from pain and bleeding, improved comfort during bowel movements, and better quality of life. Learn more
Before-and-after
Before-and-after results commonly show reduced swelling, symptom improvement, and restoration of normal anal function. Learn more
Frequently Asked Questions
1. What are piles (hemorrhoids)?
Piles are swollen veins in the lower rectum or anus that develop due to increased pressure and strain in the area.
2. What causes piles to develop?
Common causes include chronic constipation, prolonged sitting, straining during bowel movements, pregnancy, obesity, and low-fiber diets.
3. Are piles a serious medical condition?
Piles are usually not serious, but they can cause discomfort and complications if left untreated.
4. What are the common symptoms of piles?
Symptoms may include rectal bleeding, itching, pain, swelling around the anus, and discomfort during bowel movements.
5. What is the difference between internal and external piles?
Internal piles develop inside the rectum and are often painless, while external piles form outside the anus and may cause pain and swelling.
6. Can piles go away on their own?
Mild piles may improve with lifestyle changes such as increased fiber intake and proper hydration.
7. How are piles diagnosed?
Diagnosis usually involves a physical examination and, in some cases, additional tests to assess internal hemorrhoids.
8. What lifestyle changes help prevent piles?
Eating a high-fiber diet, drinking enough water, exercising regularly, and avoiding prolonged sitting can help reduce the risk.
9. When should I seek medical attention for piles?
Medical evaluation is recommended if there is persistent bleeding, severe pain, or symptoms that do not improve with basic care.
10. Can piles return after treatment?
Yes, piles can recur if preventive measures such as healthy bowel habits and proper diet are not maintained.